Conference Presentation
AI software leverages information in DBT to help identify cancers with limited or no visibility on FFDM
SBI-ACR BREAST IMAGING SYMPOSIUM 2023
Brittaney Everitt, MS
May 5, 2023
Purpose
Research comparing digital breast tomosynthesis (DBT), and full field digital mammography (FFDM) has shown that many radiologists have improved cancer detection when reading DBT, in part due to increased lesion visibility. AI models for breast cancer detection in screening mammography, including several FDA-cleared products, have also shown performance improvements on DBT. Yet, there is limited data available directly comparing FFDM to DBT in the same patient concurrently. We sought to evaluate how frequently cancer lesions are only visible on DBT relative to FFDM and to explore whether AI takes advantage of DBT information to identify lesions.
Materials and Methods
Exams were retrospectively collected from 834 women, 87 with screen-detected biopsy-confirmed cancer, who underwent combined DBT and FFDM screening mammography at 9 centers in the USA. We evaluated the 87 cancer exams using custom-built categorical AI software designed to detect suspicious findings on both DBT and FFDM. The AI output categories were: Minimal, Low, Intermediate or High, corresponding to ~25%, ~50%, ~20%, and ~5% of a screening population, respectively. An MQSA-qualified radiologist with >25 years of experience then reviewed all exams where the AI category was lower for FFDM than DBT. Blinded to the AI results, the reviewer assessed in each exam how visible the cancer was on FFDM relative to the DBT images.
Results
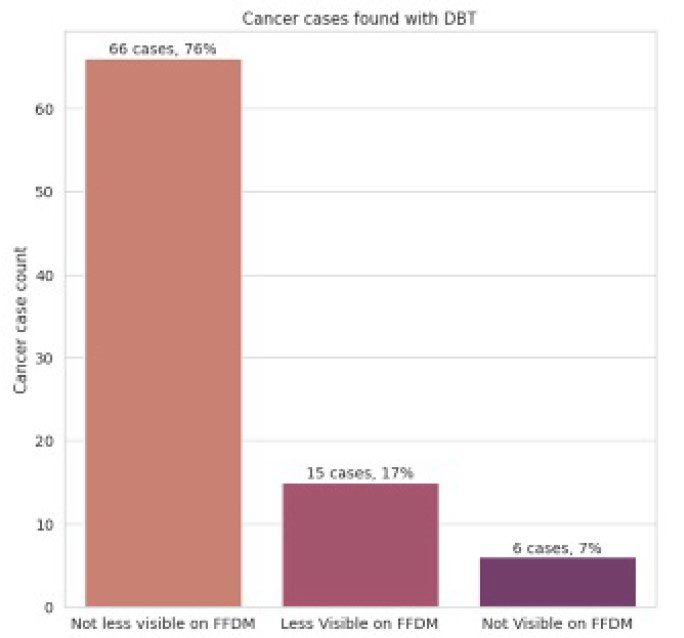
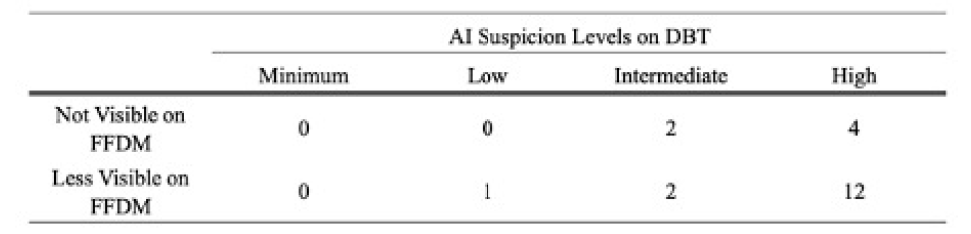
39 exams had a lower AI category on FFDM than DBT. Of these, 6 cancers were deemed not visible on FFDM, 15 cancers were less visible on FFDM than DBT, 17 exams had cancers equally visible on FFDM and DBT and 1 had a cancer deemed more visible on FFDM than DBT. 20 of the 21 cancer cases where the expert deemed the cancer not visible or less visible on FFDM were categorized by AI high or intermediate suspicion based on DBT images (Intermediate: 4, High: 16); the remaining cancer was categorized as Low.
Conclusion
Using a direct comparison of the same cancers in the same patients at the same time, ~7% of cancers visible on DBT were not visible on FFDM and ~17% were less visible on FFDM than DBT. For these cancers not visible or less visible on FFDM, the AI successfully utilized the DBT images to identify cancers.
Clinical Relevance
DBT is effective at visualizing cancer lesions that are often not visible on FFDM and AI software can utilize the additional information in DBT images to help identify cancers that are not visible or less visible on FFDM.
Figure 1
Number of cancer cases based on lesion visibility on FFDM and DBT
Table 1
AI suspicion levels on DBT images when lesions were not visible or less visible on FFDM.